ON-SITE REPORTING FROM IDF 2019, BUSAN
Diagnosed with type 2 diabetes a decade ago, Corinna Cornejo is a patient advocate and blogger who focuses on health policy and developments in digital healthcare without losing sight of their potential impact on real people's lives. Corinna blogs at https://type2musings.com/ and can be found on Twitter and Facebook as @Type2Musings.
The opinions presented in this blog post are those of the author and may not represent the opinions of Ascensia Diabetes Care.
Ascensia have paid Corinna Cornejo an honorarium for her services as a guest reporter. Ascensia did not provide any financial support for Corinna Cornejo to attend the International Diabetes Federation Congress 2019 in Busan, Korea.

-
Flourishing with Diabetes: Notes from the 2019 IDF Congress
-
-
What if we moved away from a “machine-focused” approach to diabetes care and education toward a “human-focused” approach in diabetes care and education?
It wasn’t just the tech talks at the 2019 IDF Congress in Busan that were calling for a new way of thinking about diabetes. Many of the talks about treatment and education also presented alternative ways of thinking and new approaches.
One of the most compelling talks was A Flourishing Approach: Moving from “machine” to human-based diabetes care and education delivered by Riva Greenberg, CHC, DPE, CA, HR, IS, AU, PWD, JOU, WF, CDCA.
What is machine-based thinking?
In her talk Ms. Greenberg characterizes today’s approach to diabetes management as being largely based on “machine” values. Steeped in the history and experience of the Industrial Revolution, the machine approach to health in general (and diabetes in particular) strives for accuracy and perfection. It sets forth its standards in the form of best practices. It looks at anything that doesn’t embody perfection or meet its standards as broken or defective. It assumes cause-and-effect. And it demands control.
You don’t need to look at diabetes care for very long before seeing the influence and impact of a machine-based mindset.
The aim of well-managed diabetes is to control BG levels. What we eat causes our BG levels to rise. And so does lack of sleep, mental stress, and certain kinds of physical exertion, etc. Best practice for type 2 diabetes at diagnosis is to prescribe metformin and advise lifestyle change. We download our BG meter data, look for anomalies among the readings, and then question how these failures occurred.
The problem with the machine-based approach is two-fold. First of all, humans don’t operate in the same manner as machines. Our physical and mental systems are much more complex and varied. Secondly, the machine-approach sets people up for failure. Any person who has found themselves staring at a number on their BG meter and wondered how that happened can confirm this.
The machine-based approach puts people with diabetes in a negative loop. It often starts with a BG reading or an A1C test result that is out of the target range. Soon after a question follows. How did that happen? Why is that there? What did/didn’t you do? There is no clear cut answer to any of these questions, so feelings of reproach begin to appear, followed by the admonition to “try harder.” So, the person tries again. And “fails” again. And is told to “try harder” again. Eventually, all hope and motivation are drained away and the person stops trying all together.
How is the human-based approach different?
Taking a human-based approach puts aside industrial metaphors and calls upon the wisdom and knowledge found in a set of sciences not often considered in the context of diabetes. It takes into account neuroscience, salutogenesis, and social psychology.
Neuroscience is the study of the nervous system and its impacts on a person, and how they experience and respond to the world. It looks beyond the physical aspects of the nervous system to understand the behaviors and beliefs that spring from the responses of a person’s nervous system. For example, neuroscience shows us how and why a person’s sense of hearing shuts down when they are under stress. It also shows us the long term cognitive impacts of physical and/or psychological trauma.
Salutogenesis is an approach to health aimed at fostering those things that encourage and support health, instead of discouraging disease. It focuses on the resources and capacity to generate health present in the person. Salutogenesis conceptualizes health as a continuum that we each occupy somewhere between total illness and total health, not the presence or absence of health.
Social psychology looks at the impact social environments and group interactions have on the individual and their behavior. It looks at how a person sees themselves in relationship to the group, perceives cultural norms, and how that shapes their behaviors and beliefs. These perceptions can result in feeling supported and encouraged, or rejected and stigmatized, or somewhere in-between.
With these disciplines as its basis, a human-values approach asks questions and makes assumptions that are very different from the machine-value approach.
It asks, “What’s possible?” and looks for good enough, in place of perfection. It accepts variation in place of the ideal, understanding that a person’s history and circumstances influence their actions. It sees the individual and their health as complex and non-linear instead of looking for a direct cause-and-effect relationship between, say, enjoying a family meal and the next BG reading. It’s approach is to navigate the individual’s state of health by probing for readings then responding in an individualized manner instead of relying on standard, codified approaches. It’s an approach that honors the individual and their beliefs, capabilities, and community.
This flourishing approach is based on the individual’s strengths. It looks for what’s working and how can that be encouraged to grow and spread to other aspects of their health. It’s (human) relationship-based and encourages cooperative decision making and solution building.
Flourishing is not an either-or approach
In moving toward a more human-based approach to diabetes care and education, there’s no suggestion that the machine-approach (and the medical devices it has generated) should be abandoned. On the spectrum of health, both approaches serve distinct purposes and can work together to generate outcomes that work best for the individual person living with diabetes, encouraging them to flourish overall and not focus on a few, specific data points to measure their health.
-
-
Diabetes Tech: Notes from the 2019 IDF Congress
-
-
- High cost of diabetes tech
- Patient access to diabetes tech varies widely
- Education needed by patients, caregivers, and medical professionals to effectively use diabetes tech isn’t widely available
- Regulatory requirements and approvals vary widely
- Integrating new approaches and technology into established clinical practices is challenging and takes time
- Managing data overwhelm and fatigue experienced by patients, caregivers, and medical professionals
- Managing the medical waste generated by diabetes technology
- Pre-planning for technological failures and outages
“We now have all the components to automate diabetes care.”
—Anastasia Albanese-O'Neill, A.R.N.P., Ph.D., C.D.E.
My ears perked up when I heard Dr. Anastasia Albanese-O'Neill, Ph.D. make this declaration at the 2019 IDF Congress in a session about improving diabetes care with the help of technology.
Then my logical mind stepped in to parse what I heard.
We have all the technological components. She was referring to CGMs, insulin pumps, and algorithms. As for the diabetes care, it’s focused primarily on monitoring glucose levels and dosing insulin.
There’s no denying that diabetes technology has made remarkable progress in our lifetimes.
Since the 1970s BG monitoring has gone from trying to match the color of a urine-saturated strip to a chart in order to identify a range of BG levels, to then getting a three-month view of BG levels through the A1C blood test, to now being able to read a specific numerical reading paired with a trend line on a smartphone in nearly real time. Insulin therapy has gone from one or two shots a day of NPH and animal-origin insulin, to multiple daily injections (MDI) of purified insulin, to continuous subcutaneous insulin infusion therapy (i.e., insulin pump therapy).
Where will diabetes tech take us next?
The promise and path forward for diabetes tech were recurring themes across the tech-focused sessions I attended in Busan.
No Blind Spots: The promise of diabetes tech
The promise of diabetes tech has always been more data and more complete coverage. The tech developments discussed at the IDF Congress called for more of the same.
Today’s CGMs and insulin pumps record a 24/7 datastream of BG levels and insulin dosing, eliminating blind spots in tracking and reporting. The expectation has been that more data will give better insights and lead to better diabetes care decisions. Better meaning few or no hypoglycemic or hyperglycemic episodes. Ultimately meaning fewer or no diabetes complications.
With the CGM and insulin pump now available, how can we maximize the impact of diabetes tech?
Time In Range: The path forward for blood glucose management
Across the board Time In Range (TIR) was presented as the new, more accurate way to look at BG management. Bolstered by the International Consensus on Use of CGM, released in mid-2019, this new standard goes beyond the three-month average reported in the A1C to present a more nuanced picture of a person’s BG levels.
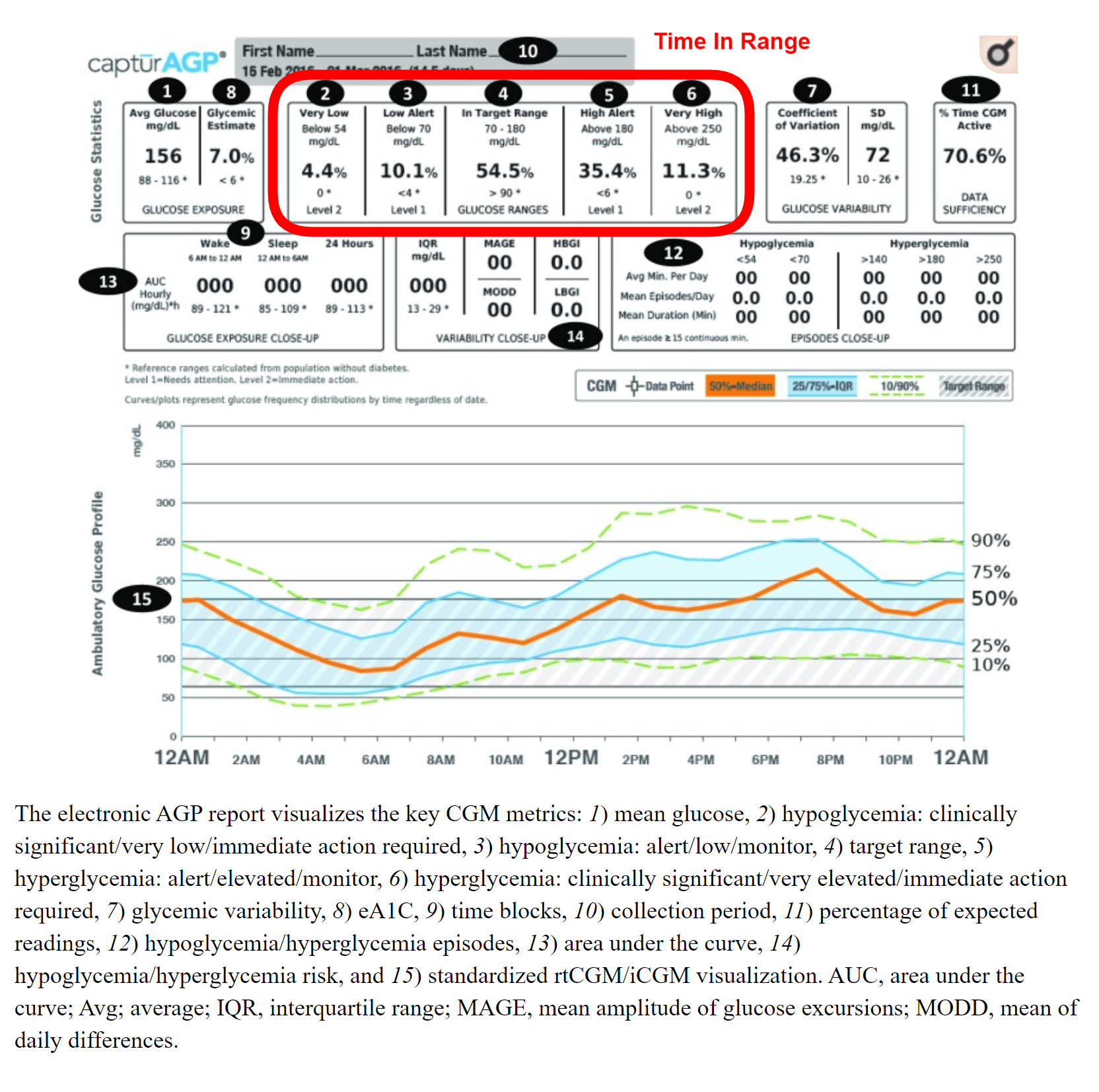
Sample EHR highlighting Time In Range statistics | © 2017 by the American Diabetes Association
Made practical with the use of CGM, TIR reports the percentage of time the person’s BG levels were within a clearly defined target range. For most people the TIR target is 70% or more of time with BG levels between 80 mg/dL and 180 mg/dL (4.4 mmol/L to 10 mmol/L).
By adopting TIR as the new standard, tracking and reporting can become more detailed and accurate. Diabetes care will focus on consistently keeping BG levels within defined boundaries and not assuming that highs and lows will balance each other out over time.
Looping: The path forward for insulin dosing
Closed loop was touted by several speakers as the future for managing insulin dosing.
These algorithm-driven systems make it possible for an insulin pump to dose insulin in response to a BG level reading read from a CGM in real time. The software algorithm behind looping ensures consistent insulin dosing with less hands-on management by the person.
In less than a decade development of looping systems have gone from patient-driven DIY artificial pancreas projects made from off-the-shelf medical devices to a specific FDA-approved medical device that provides a hybrid closed loop system. Then, I came home to the news that the FDA has just approved its first interoperable automated glycemic controller device capable of working with various combinations of FDA-approved medical devices.
This makes me think that the future in diabetes tech is happening now, at least for some.
Can the Promise of Diabetes Tech Be Fulfilled?
The technical components to automate much of diabetes care do exist and are available to those who can afford them. But we are nowhere close to having that tech widely available. Barriers still exist.
Several of the presenters acknowledged these barriers. Sadly, none suggested clear paths for how to remove them.
Many of the barriers to adopting cutting-edge diabetes tech are familiar. They include:
We are seeing some progress in addressing these barriers by some regulators and large healthcare systems. However, for the vast majority of people with diabetes in the world there is limited or no access to well-established diabetes tech like BG meters, let alone anything that is cutting-edge. For these people the promise of diabetes tech remains beyond reach.
-
ASCENSIA
MENU
QUESTIONS ABOUT THIS SITE?
If you have any questions about the latest available blood glucose solutions, contact Ascensia Diabetes Care in your country. Visit contact.ascensia.com for a full listing of countries.
Questions or comments about this website, please CLICK HERE.
QUESTIONS ABOUT THIS SITE?
If you have any questions about the latest available blood glucose solutions, contact Ascensia Diabetes Care in your country. Visit contact.ascensia.com for a full listing of countries.
Questions or comments about this website, please CLICK HERE.
Please note that not all products are available in every country.
Ascensia Diabetes Care, the company that brings you CONTOUR® and Eversense® products.
Ascensia, the Ascensia Diabetes Care logo and CONTOUR are trademarks of Ascensia Diabetes Care Holdings AG.
© Copyright 2024 Ascensia Diabetes Care Holdings AG. All rights reserved.
Last updated: July 2022. Code: G.DC.01.2016.37920
Please note that not all products are available in every country.
The company that brings you CONTOUR® products now has a new name. Introducing Ascensia Diabetes Care.
Ascensia, the Ascensia Diabetes Care logo and CONTOUR are trademarks of Ascensia Diabetes Care Holdings AG.
© Copyright 2017 Ascensia Diabetes Care Holdings AG. All rights reserved.
Last updated: July 2016. Code: G.DC.01.2016.37920


